Background
Fractures of the talus can be divided into types based on the 3 main anatomic divisions of the talus: body, neck, and head. Fractures of the body of the talus are further subdivided based on whether they traverse the main portion of the body or are fractures involving the talar dome, lateral process, or posterior process. Mechanisms of injury, treatment, and prognosis of the different types of talar fractures are markedly dissimilar.

Talar body fracture, anteroposterior radiograph. There is a sagittally oriented fracture through the body of the talus and disruption of the tibiotalar and subtalar joints. The injury was from a motor vehicle accident.

Talar body fracture, anteroposterior radiograph. There is a sagittally oriented fracture through the body of the talus and disruption of the tibiotalar and subtalar joints. The injury was from a motor vehicle accident.

Fractures of the lateral and posterior processes of the talus, axial computed tomography (CT) scan. These fractures were associated with a talar body fracture.

Fractures of the lateral and posterior processes of the talus, axial computed tomography (CT) scan. These fractures were associated with a talar body fracture.
Frequency
United States
Talus fractures reportedly make up 3-5% of foot fractures. However, they are probably underreported, especially osteochondral fractures and fractures of the lateral and posterior processes of the talus, which are radiographically difficult to detect.
Approximately 50% of fractures of the talus involve the talar neck. The most common fracture of the talar body is the osteochondral fracture, followed by fractures of the posterior and lateral processes. Fractures of the main portion of the talar body and of the talar head are uncommon.
Mortality/Morbidity
Fractures of the talus can lead to avascular necrosis (AVN), arthritis, and, when unrecognized, chronic pain and nonunion. These develop as follows:
- AVN of the body of the talus - This condition develops primarily after a displaced fracture of the talar neck—which disrupts the blood supply to the talar body—has occurred. The risk of AVN can be estimated by the Hawkins classification (discussed below). An adequate blood supply to the talus can be inferred when a Hawkins sign is present (see Image below and Image 24 in Multimedia).1,2,3

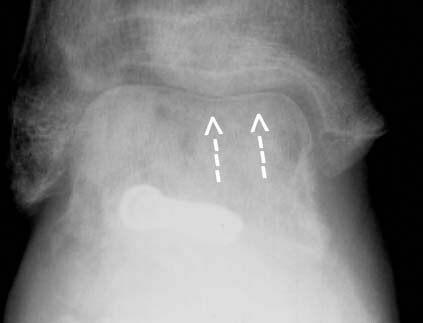
Anteroposterior radiograph. Following open reduction and internal fixation of a Hawkins type II fracture, a Hawkins sign (arrows), indicating intact vascularity, is seen over most of the talar dome. Laterally, however, the Hawkins sign is absent. The lateral portion of the dome is sclerotic, representing a small focus of avascular necrosis that has developed there.
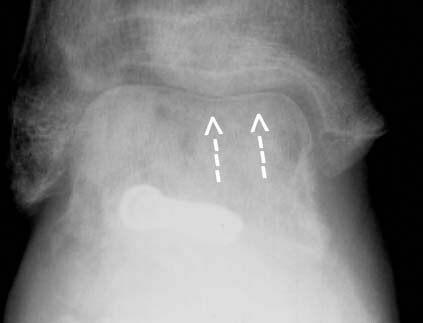
Partial Hawkins sign, anteroposterior radiograph. Following open reduction and internal fixation of a Hawkins type II fracture, a Hawkins sign (arrows), indicating intact vascularity, is seen over most of the talar dome. Laterally, however, the Hawkins sign is absent. The lateral portion of the dome is sclerotic, representing a small focus of avascular necrosis that has developed there.
- Arthritis - A common complication following talar fracture, talus-related arthritis can involve the tibiotalar, subtalar, or talonavicular joints. Exact surgical reduction is a goal in the prevention of posttraumatic arthritis.
- Chronic pain and nonunion - These complications are not infrequent following undetected talar fractures. Osteochondral fractures of the talar dome, posterior process fractures, and lateral process fractures may be difficult to detect radiographically; clinically, they may be mistaken for ankle sprain. Patients with an undetected talar fracture present later with chronic pain and often with nonunion of the lateral or posterior process, at which time the fragment may require excision. Undetected osteochondral fractures may progress to loose bodies within the joint.
Age
Fractures of the talar dome, lateral process, and posterior process occur primarily in young athletes. Other talar fractures occur at any age, usually as a result of motor vehicle accidents or falls from a height.
Anatomy
The talus is unique in that no tendons attach to it. It is held in place by ligamentous and bony structures. The talus articulates superiorly with the tibia, medially and laterally with the medial and lateral malleoli (respectively), inferiorly with the calcaneus, and anteriorly with the navicular.The talus can be divided into 3 main parts: body, neck, and head.
Body
The body, which is the largest portion of the talus, is divided into 4 parts, as follows:
- Dome - The dome articulates with the tibial plafond. Although termed a dome, it is shaped like a pulley, being convex from front to back but slightly concave from medial to lateral. Plantarflexion and dorsiflexion take place at the tibiotalar joint.
- Central portion - The central portion has articular facets medially and laterally that articulate with the malleoli, as well as an inferior articular facet that articulates with the posterior facet of the calcaneus. Inversion and eversion, as well as plantarflexion and dorsiflexion, take place at the posterior subtalar joint.
- Posterior process - The posterior process of the talus projects from the posteroinferior aspect of the talar body and is nonarticular.
- The flexor hallucis longus (FHL) tendon courses between medial and lateral tubercles of the posterior process. Fractures of the posterior process can affect the FHL.
- The posterior process of the talus can be present as a separate ossicle, the os trigonum.
- Lateral process - The lateral process of the talus protrudes beneath the tip of the fibula. On a lateral radiograph, it forms a wedge shape at the anterior aspect of the posterior subtalar joint, with the apex of the wedge pointing inferiorly. The posterior subtalar facet extends into this region, and fractures of the lateral process often involve that joint.
Neck
The neck of the talus is roughly cylindrical in shape and is considerably narrower than the body. The talar neck is separated from the calcaneus by the fat-filled sinus tarsi.
The main blood supply of the talar body enters the talar neck from the sinus tarsi (a fat-filled space between the talar neck and the calcaneus) and proceeds retrograde to supply the talar body. Thus, fractures of the talar neck can compromise the vascularity of the body of the talus.
Head
The head of the talus is convex anteriorly and articulates with the navicular. Abduction and adduction are the primary motions at the talonavicular joint.
Presentation
The mechanism of injury and clinical presentation of each of the 6 main types of talar fracture vary markedly. For purposes of conciseness and clarity, they are discussed below in the Radiograph/Findings section.
Preferred Examination
Plain radiographs of the foot and ankle are used to diagnose talar fractures. The views obtained depend on the particular fracture and are discussed separately (see below). Computed tomography (CT) scanning is used to evaluate displacement and to plan surgery. CT scanning and magnetic resonance imaging (MRI) are used to diagnose clinically occult fractures.4,5,6
Limitations of Techniques
A close, directed scrutiny of radiographs is needed to detect many talar fractures. Fractures of the lateral process are especially difficult; they may be visible on the anteroposterior (AP) ankle radiograph, the Broden view (45° internal oblique), or only on the lateral view of the foot.
CT scanning and MRI are used to detect radiographically occult fractures of the talus but must be performed with high resolution and attention to patient positioning. MRI can be difficult to interpret if planes orthogonal to the long axis of the talus are not used. CT scanning should be performed in the coronal and axial planes; otherwise, fractures may be missed.
Info found at:http://emedicine.medscape.com/article/396568-overview
 Ready in:
Ready in: